Your experts for skin transplantation
Hier erläutern wir Ihnen die verschiedenen Möglichkeiten der Hautverpflanzung. Lernen Sie die Vor- und Nachteile der SkinDot-Transplantation, Spalthaut-Transplantation, Kulturhautverfahren im Labor gezüchteter Zellen und die Möglichkeiten des Ersatzes tieferHautschichten (dermale Ersatzverfahren) kennen. Welche Hauttransplantation eignet sich wofür?
Ask our experts
Warning
They may contain disturbing photos.
Dermal replacement procedures
For deep wounds with complete loss of all skin layers, a collagen-based dermal substitute can be grafted into the wound. This collagen matrix acts as a skin shifting layer. A thin layer of skin must then be transplanted over the dermal substitute.
Culture skin method
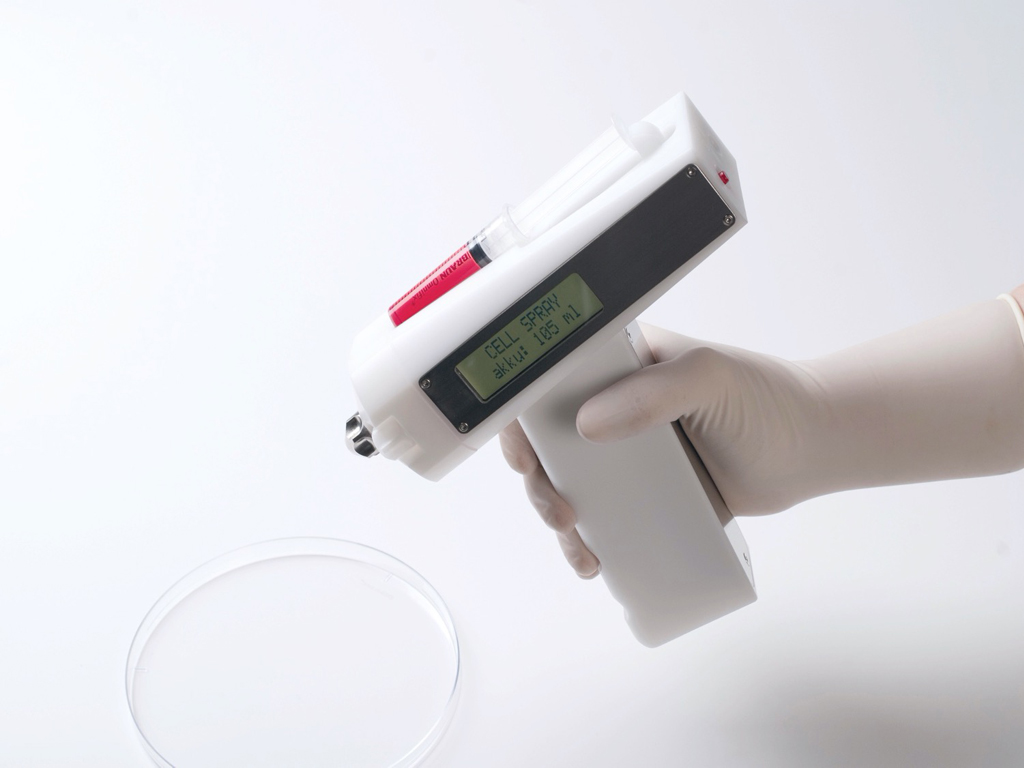
Since the 1980s, skin cells can be grown in the laboratory. The skin cells grown (cultured) in the laboratory can be inserted into the wound as cell layers or sprayed on the wound.
Split skin graft
For extensive burns and very superficial wounds, so-called split-thickness skin grafting is the treatment of choice. Split skin consists of an ultra-thin skin graft of the thickness of only 0.2 mm.
SkinDot skin graft
In the case of a deep wound with a loss of the entire skin, skin replacement with so-called full-thickness skin provides the best result. Full-thickness skin grafts are very stable due to their dermal shifting layer and contain all skin appendages.
Culture skin process and skin cell cultivation
Since the 1980s, cultured skin cells (keratinocytes and fibroblasts) can be routinely used in the care of severely burned patients. The possibilities range from so-called keratinocyte sheets (three-dimensional cell structures) to cell suspensions. In cell suspension, cells grown in the laboratory are sprayed onto the wound.
Unfortunately, the possibilities of cell cultivation fall short of expectations. For example, although it is possible to individually grow the different cell types required for a full-thickness skin substitute in the laboratory. Unfortunately, however, it is not yet possible to assemble the various skin cell types into a functional organ in the foreseeable future. The complexity of the skin organ has long been underestimated. In addition, the cells are very sensitive to infection during the up to three weeks of cell cultivation in the laboratory and very sensitive to pressure and touch after transplantation. Because of this pressure sensitivity, they cannot be transplanted to areas of the body that can bear weight.
In the long run, ultra-thin, very sensitive skin grafts result, which are (still) miles away from a full-layer skin replacement.
Cultured Epithelial Autograft (CEA)
This term, which is firmly established in medical care, refers to cells cultivated in the laboratory (cultured = cultivated in the laboratory, epithelial = epidermal = top layer of skin, autograft = graft from the patient’s own body tissue). CEA grafts, which are now routinely used worldwide, consist of a multilayered layer of the patient’s own skin cells (keratinocytes)
.
The advantages lie in the virtually unlimited number of cells that can be cultured. In the context of superficial wounds in which the subcutis (dermis) is preserved. CEA grafts lead to cosmetically flawless postoperative results. However, they are thus suitable only for replacement of the thin epidermis. In contrast, the results are extremely poor, both functionally and aesthetically, when the subcutis (dermis) is lost and when transplanted to fat or muscle tissue. It was not until work by Cuono in 1987 and Hickersen in 1994, who initially transplanted cadaveric skin into the wound bed, that better clinical results were obtained with CEA. Thus, it is important to introduce subcutaneous components (derived from cadaveric skin) into the wound bed prior to the use of CEA grafts in order to increase the healing rate of the laboratory-grown cells. This is accomplished in the case of subcutaneous loss primarily by transplanting cadaveric skin prior to application of the laboratory-grown skin cells. The cadaver skin heals due to the immunosuppression associated with the severe burn injury and can serve as a temporary skin substitute for a 3-4 week period. During this time, the skin cells are cultured in the laboratory. In this way, in several surgical steps, it is possible to successfully transplant the cultured cells.
Whenever possible, cultured skin procedures are performed in combination with split skin. Due to the shear forces on the mechanically stressed areas of the body (back of the head, buttocks, back), the expanded autologous split skin is transplanted, if available. For this purpose, autologous skin grafts are applied to the mechanically stressed wound areas, e.g. using the special technique developed by Meek or as wide-meshed mesh graft grafts with an expansion of 1-3 to 1-6. Skin cells grown in the laboratory are transplanted to the areas not affected by shear forces. This procedure can also be used to treat extensive burns of more than 90 percent body surface area, as long as the patient survives the first few days of severe burn trauma.
| CEA Sheet | Advantage | Disadvantage |
|---|---|---|
| Skin quality of the graft | Poor, because no skin appendages in the graft, no stem cells present, no dermal shift layer, consisting of keratinocytes only. | |
| Healing of the graft | Poor, as very sensitive to pressure | |
| Scarring | Low | |
| Donor area | Small area removal for cell cultivation possible on all remaining healthy skin areas | |
| OP-Zeit | Complicated technique, long manufacturing time of the transplants in specially approved institutes necessary | |
| Costs | Very high cost, one sheet (10 x 10 cm = 400 Euro) |
Cultured Epithelial Autograft (CEA) as suspension
The laboratory-grown skin cells can not only be transplanted as a three-dimensional matrix (sheet), but can also be sprayed onto the wound. Hunyadi et. al. were the first to apply laboratory-grown skin cells (keratinocytes) in droplet form to chronic wounds.
Later, technical inventions were added that allowed cell suspensions to be sprayed onto the wound, increasing the uniform distribution of cells on the wound compared with grafting by pipetting. Since the skin cells grown in the laboratory do not need to accumulate in multiple layers of the three-dimensional matrix in this method, the method of growing cells for spraying is much easier. When the skin cells are grown in the laboratory, they only need to be grown for a few days. Another method is not to grow the skin cells, but to obtain the skin cells directly from a small piece of skin during surgery. In this method, the skin cells are not multiplied or cultured, but the small piece of healthy skin is dissolved into individual cells. Then, the cells obtained from the small piece of healthy skin are sprayed onto the wound.
However, this modern method also has the disadvantage that only the epidermis can be replaced. In addition, parts of the subcutis (dermis) must be present in the wound so that the sprayed cells can grow in the wound. The best known commercially available product for cell spraying without cultivation in the laboratory is Recell®. The advantage of is Recell® is rapid and safe wound closure in very superficial skin defects, especially superficial burns and scalds in the facial area.
.
The different commercially available CEA are listed in the table. Products available in the U.S. are not available in Europe due to the complex approval process for cell-based products, which fall not only under the Drug Act, but additionally under the much stricter Transplantation Act.
| Product name | Cultured Epithelial Autografts (CEA) | |
|---|---|---|
| Epicel® | Genzyme Biosurgery | Cultured autologous epidermal human keratinocytes, grown using mouse fibroblasts, Sheet. |
| Myskin® | Celltran Ltd | Cultured autologous epidermal human keratinocytes, cultured using irradiated mouse fibroblasts, sheet |
| Epidex® | Euroderm GmbH | Cultured autologous epidermal human keratinocytes, cultured using mouse hair follicle cells, sheet. |
| Keratinozytensheet | Deutsches Institutu für Zell- und Gewebetransfer (DIZG) | Cultured autologous epidermal human keratinocytes, grown using collagen-coated cell culture flasks, Sheet. |
| Keratinozytensuspension | Deutsches Institut für Zell- und Gewebetransfer (DIZG) | Cultured autologous epidermal human keratinocyte suspension, cultured using collagen-coated cell culture flasks, suspension. |
| Recell® | Clinical Cell Culture Ltd | Autologous intraoperatively prepared autologous human mixed cell suspension. |
Your attending physician is not yet familiar with the new, innovative SkinDot procedure? Please inform him/her about the possibility of treating your skin wound with the new SkinDot procedure. We will be happy to advise you and perform the SkinDot procedure on you (if indicated). We look forward to hearing from you!
Skin Transplantation beyond
Skin Transplantation 2.0