What is SkinDot?
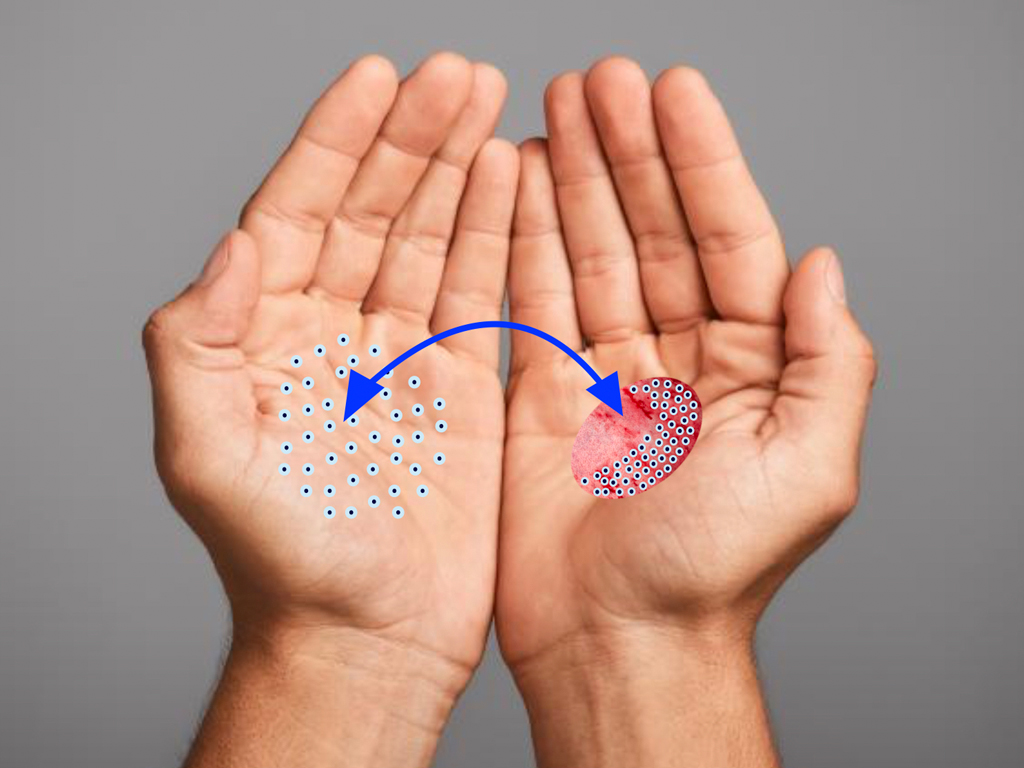
SkinDot opens a new, innovative therapeutic approach for wound care of IIb° – III° burn wounds, acute full-thickness defect wounds, chronic wounds as well as in surgical scar correction. In this approach, 1-3 mm full-thickness skin islands are harvested, implemented into a matrix, and the matrix with the islands is transplanted onto the wound. The result is a stable and resilient autologous skin substitute.
Warning
They may contain disturbing photos.
The best skin replacement is our goal
Nothing is better than the original. Injured skin is best replaced with healthy skin. Through years of experience in burn surgery, we have developed a new surgical procedure in which millimeter-sized islands of healthy skin are transplanted into the wound area. These countless grafted islands of skin grow together to form new, healthy skin in the wound area.
In the process, islands of skin are harvested that contain all layers of skin, including stem cells, and inserted into the wound.
After more than 10 years of intensive medical research by the research association and numerous publications between the University of Lübeck, the Technical University of Lübeck and the Unfallkrankenhaus Berlin, we have developed the new, innovative transplantation procedure SkinDot for you. For the first time worldwide we offer the SkinDot procedure for our patients.
What is SkinDot?
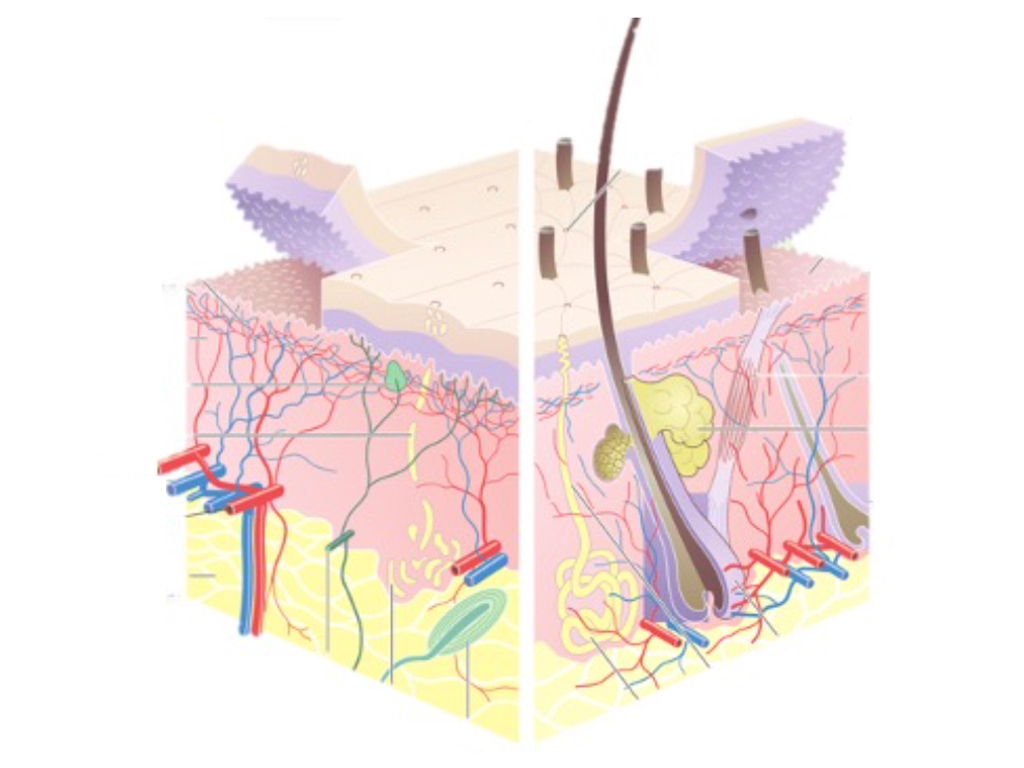
Commonly, skin grafting in acute and chronic wound care and burn surgery consists of transplantation of the upper layer of skin. However, this standard procedure does not result in the replacement of the deep layers of skin.
However, these deep skin layers are indispensable as a displacement layer and carrier of skin appendages such as hair, sweat and sebaceous glands, and nerve receptors for pressure, vibration and temperature sensation, and thus for the quality of the transplanted skin.
Until now, these deep skin layers could only be transplanted at great expense and not over a large area. Only the coverage of 2-3% of the skin surface was possible.
A skin substitute based on cultured skin cells in the laboratory is also currently not developed far enough to replace the deep skin layers. In addition, cell cultivation is costly, lengthy and fraught with complications.
Due to SkinDot, a new transplantation procedure is now available for the first time in the world, through which the deep skin layers can be restored in a single operation without cell cultivation.
SkinDot advantages for patients
Current skin grafting:
- Kein großflächiger Ersatz der tiefen Hautschichten möglich – Fast ausschließlich oberflächliche und dünne Hauttransplantate werden verpflanzt.
- Limitierte Hautentnahmestellen für Haut, die alle Hautzellen bzw. Hautanhangsgebilde enthält.
- Nur 2-3% der Körperoberfläche kann durch tiefe Hautschichten ersetzt werden
- Funktionseinschränkende Narbenbildung besonders über Gelenkflächen
- Deutliche Stigmatisierung durch Narbenbildung bei exponierten Wundarealen
The new SkinDot skin graft:
- Die neue SkinDot Technologie ermöglicht die Transplantation tiefer, gesunder Hautschichten
- Durch die verpflanzten Hauptinseln im Millimeterbreich resultieren kaum Narben
- Sofortige intraoperative Verfügbarkeit ohne Vorbereitung oder Voroperationen
- Die Hautinsel Gewinnung ist überall am Körper möglich, insbesondere an nicht sichtbaren Körperstellen
- Kosmetisch günstiges operatives Ergebnis, vor allem geeignet für Gesicht und Hände
- Keine Stigmatisierung durch entstellende Narben nach Brandverletzung
- Vermeidung funktionseinschränkende Hautnarben nach schweren Hautverletzungen
Optimal wound therapy through skin grafting
.
Skin grafting is the transplantation of skin to cover skin defects after loss of the skin mantle from injury. In healthy individuals, after superficial or very small skin defects, the skin is able to regenerate itself and replace wounds with fully functional tissue. In the case of larger wounds and/or various underlying diseases (e.g. diabetes mellitus, vascular diseases, immunosuppression, etc.), wound healing can be very slow and protracted, resulting in severe scarring or a chronic wound. In superficial wounds, the skin heals starting from the wound bed because so-called stem cells are preserved in the deep layers of the skin. In deep wounds, especially deep burn wounds, the deep skin layers are damaged, so that wound healing starts only from the wound edge. This results in extremely protracted wound healing with the risk of infection and chronification. The longer a wound is open, the higher the risk of infection, since the skin is a barrier against germs (bacteria, viruses, fungi). Especially in patients with pre-existing conditions and burn victims, this wound infection can lead to blood poisoning (sepsis). Therefore, prompt wound closure by skin grafting is necessary for larger wounds and burn patients. There are several methods of skin grafting, but each involves a surgical procedure under anesthesia.
SkinDot – Optimal therapy for burn wounds
Depending on the depth of the burn (burn or scald), different layers of skin are injured. Superficial burns and scalds are usually characterized by blistering. This superficial skin injury heals within a period of approximately 14 days.
The superficial burn with blistering on the fingers is one of the most common injuries in humans, everyone has been burned on their fingers. If the superficial burn is larger, it must be cleaned and treated by a doctor. Depending on the size of the burned body surface, an inpatient stay at a burn center may be necessary.
If deep skin layers are affected by the burn or scald, burn or scald wounds larger than about 1cm² must be treated surgically by skin grafting.
The best skin substitute after loss of deep skin layers is the transfer (transplantation) of deep skin layers from a healthy body site into the skin wound. Until now, transplantation of deep skin layers has been very limited. With the new SkinDot procedure, large-scale transplantation of deep skin layers is possible for the first time.
Optimal wound therapy for chronic wounds
In Germany, approximately one million people live with a chronic wound. Keeping track of treatment procedures for chronic wounds is sometimes difficult. However, this is due more to an ever-increasing range of medical products in the field of wound dressings and less to a paradigm shift in the underlying principles of wound therapy. Chronic wounds can be made to heal with targeted treatment of the cause of the wound, optimal wound bed preparation, and skin grafting.
A critical and guiding component of wound management in chronic wounds is clarification of the cause of the wound or the cause of impaired wound healing. Causes include vascular (e.g., venous, arterial, mixed venous-arterial), traumatic, or pressure-related, as well as infectious, metabolic (diabetes mellitus, and others), immunologic, or neoplastic. Cause therapy, such as revascularization, decompression, or pharmacologic intervention (antibiotics), can have a significant impact on the healing process. Once the cause of the chronic wound has been eliminated, defect closure is accomplished by skin grafting.
The new SkinDot procedure is excellently suited for this purpose, as deep skin layers are introduced into the chronic wound, resulting in stable wound healing.
More about wound therapy for chronic wounds
Neben der oben genannten Ursachentherapie bei chronischen Wunden ist es wichtig, ein ideales Wundmilieu für eine gute Wundheilung herzustellen. Im Mittelpunkt steht dabei die Schaffung eines Wundgrundes, der gut durchblutet, frei von totem Gewebe und Infektion ist. Zudem ist eine gute Feuchtigkeitsbalance (Kontrolle des Wundsekrets) für die Wundheilung förderlich. The following describes in detail the basic principles for creating such an ideal wound bed in the context of chronic wound therapy.
Wound cleansing: Wound irrigation and wound disinfection
Wound irrigation is used to reduce the bacterial load and remove dead cells in the chronic wound. Isotonic saline solution is best for repeated irrigation. If the wound is infected, aseptic solutions are used for wound irrigation. If the infection is persistent and dead tissue fragments are difficult to dissolve, pressure irrigation is suitable. However, antiseptic substances not only have an antiseptic effect, but can also irritate the wound. Suitable solutions for wound irrigation often contain iodine, silver or polyhexanide. Locally applied antibiotics are rarely used due to the risk of resistance formation.
Mechanical wound cleaning (Debridement)
Chronic wounds are often covered by a so-called biofilm. This biofilm consists of microorganisms that produce polysaccharides and proteins to protect themselves from the body’s immune defenses and antimicrobial substances. Typical biofilm formers include the bacteria Pseudomonas and Staphylococcus.
Mechanical wound cleansing removes these biofilms as well as dead tissue components in the wound. Debridement significantly reduces the number of bacteria in the wound, since bacteria prefer to colonize dead tissue components. The aim of debridement is to stimulate wound healing by transforming the chronic wound into an acute, bleeding wound. New endogenous defense cells enter the wound with the blood flow. Debridement should be repeated regularly depending on the extent of biofilm and dead tissue. Es gibt verschiedene Formen des Debridements, das häufigste ist die Wundreinigung mit chirurgischen Instrumenten wie Instrumenten wie Skalpell, Schere, Kürette oder scharfem Löffel. Because mechanical wound cleansing is very painful, it is most often performed under general anesthesia.
Enzymatic and autolytic wound cleansing
Enzymatic wound cleansing is very safe and has few complications, as only dead tissue is removed by the enzymes. In autolytic wound cleansing, the principle is to keep the wound moist, e.g. with hydrocolloids or hydrogels under occlusion, so that the body’s own enzymes dissolve the dead tissue components in the wound.
Biological wound cleansing
Biological debridement (also called biotherapy or biosurgery) is therapy with maggots (usually maggots of the golden fly Lucilia sericata). The live, sterile cultured maggots are placed either loosely or in a bag on the chronic wound and left for 48 to 72 hours. On the one hand, the maggots secrete a protein-dissolving secretion as part of extraintestinal predigestion that softens the dead tissue; on the other hand, the maggots feed mainly on dead cellular components and spare the healthy tissue. In addition, it is assumed that the maggot excretions have antimicrobial effects. This form of wound cleansing may seem very special at first, but it has an excellent effect on chronic wounds.
Wound dressings and dressings
While until the middle of the 20th century it was still believed that wounds healed best when air-dried, the 1960s saw a paradigm shift to moist wound treatment.
Numerous clinical studies have provided evidence that maintaining a moist wound environment is superior to dry wound treatment. Thus, the old surgical rule of thumb of “dry on dry” and “moist on moist” has been consigned to the realm of myth. The moist environment not only facilitates cell regeneration but also promotes autolytic debridement.
Zudem werden die Schmerzen beim Verbandswechsel durch das Feuchthalten der Wunde deutlich reduziert. Bei der großen Auswahl von feuchten Wundauflagen ist es heutzutage sehr schwierig, die richtige zu finden. Da es nicht eine universelle Wundauflage gibt, die für alle Wunden passt, sondern die verschiedenen Wundauflagen Vor- und Nachteile haben sollte die Wahl eine individuelle, auf die Wunde zugeschnittene Entscheidung sein.
Wundkonditionierung mittels Unterdrucktherapie
Eine moderne und äußerst effektive Therapieoption chronischer Wunden ist die Behandlung mit Unterdruck. Dabei wird nach der Wundreinigung ein Schwamm in die Wunde gelegt und mit Folie angeklebt. Anschließend wird über ein Schlauchsystem durch ein kleine Pumpe der Unterdruck erzeugt. Aufgrund der sogenannten „Mechanotransduktion“ wird durch den Unterdruck das Gewebe zum Heilen angeregt.
Definitiver Wundverschluss durch Hauttransplantation
Ist die Wunde durch eine der verschiedenen Möglichkeiten der Wundreinigung und Wundkonditionierung optimal vorbereitet, das tote Gewebe entfernt, die Infektionsfreiheit hergestellt und die Durchblutung ausreichend, kann die Hauttransplantation erfolgen. Details der verschiedenen Arten der Hauttransplantation finden sich unter dem Reiter „Hauttransplantation“ oben in der Navigationsleiste.
SkinDot – Ideal skin replacement by autologous skin grafting for burn wounds as well as acute and chronic wounds.
.
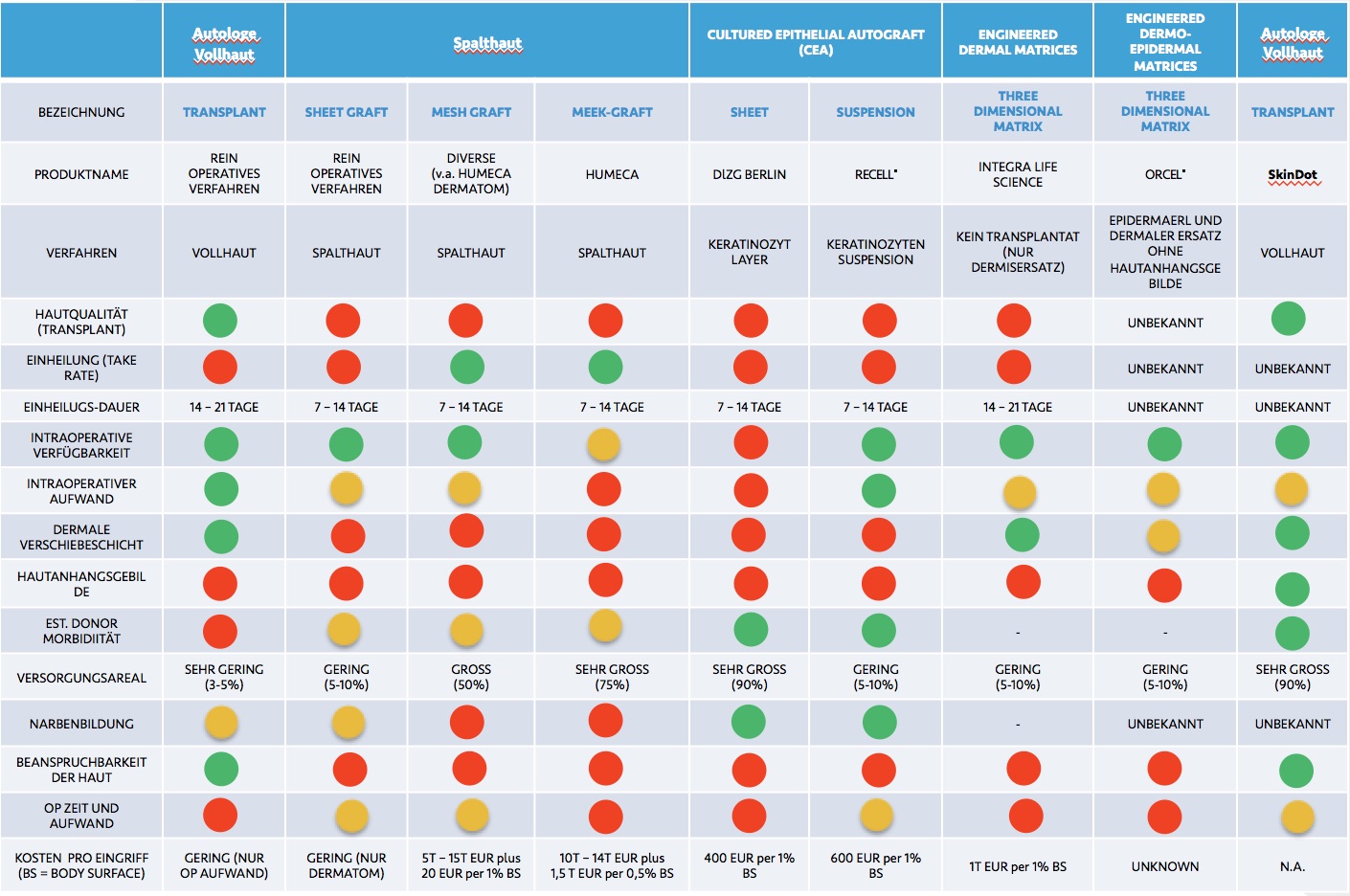
Skin Transplantation beyond
Skin Transplantation 2.0