Indications
The skin is composed of the thin epidermis and the thick dermis. The dermis represents the displacement layer of the skin. It contains all the important skin cells (sweat glands, sebaceous glands, nerves, hair roots). In the case of superficial skin loss, the deep (dermal) skin layer is completely or partially preserved, so that only a very thin (epidermal) skin layer needs to be transplanted. This thin layer of skin has a thickness of about 0.2 mm and is usually removed from the thigh. There, the skin removal creates a kind of abrasion wound, which heals on its own within 1-2 weeks. In all deep skin defects, the epidermis and subcutis are affected. Due to the loss of the dermis, transplantation of the thin epidermis alone results in a complete loss of function of the skin. SkinDot solves this problem. Through the SkinDot technique, all skin layers are transplanted in the form of 1-3 mm healthy, autologous skin islands. As a result, the lost skin is replaced by new, comparable epidermis and subcutis. For which wounds (indications) SkinDot is best suited, you can read here on this page.
Warning
They may contain disturbing photos.
Indication IIb° – III° Burn
Basically, superficial burns (grade II) heal on their own. Deep burns (grade III) require surgical wound care by skin grafting. The burned, dead tissue should be removed as quickly as possible before skin grafting to minimize an exaggerated immune response by the body and to deprive germs of a breeding ground for infection.
Therefore, prompt surgical removal of dead tissue from the burn wound within three days of the accident is now the standard therapy and most common approach in the medical management of burn wounds. Within one week to ten days at the latest after the thermal trauma, the burned, dead tissue portions should have been completely removed. In severely burned patients, these frequent surgeries are often a balancing act, as each surgical procedure carries a high risk due to blood loss. However, to avoid wound infection and the threat of sepsis, all dead tissue must be removed.
The surgical procedure consists of removing the burned skin layers until a healthy wound bed is reached. In the case of fourth-degree burn wounds that extend far into the subcutaneous fatty tissue and adjacent muscles, all deep-lying burned tissue layers are also removed.
.
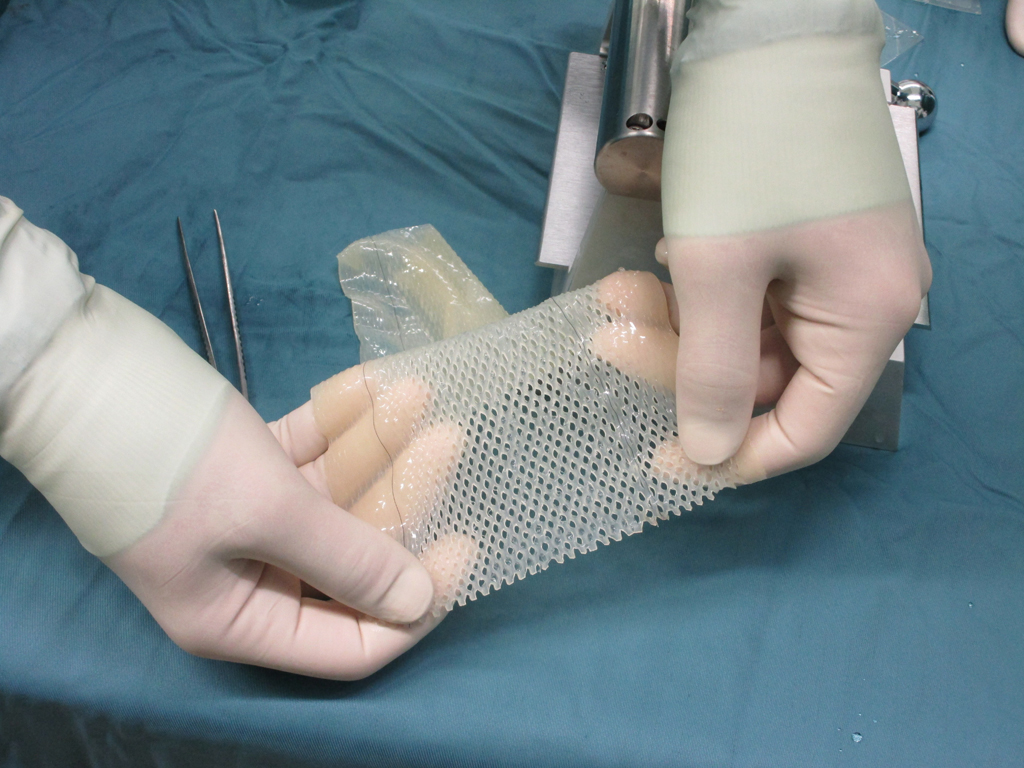
Efforts to treat burn wounds by skin grafting have been made for a long time. For example, Jack Louis Reverdin performed the first skin graft as early as 1872. The qualitatively best skin transplantation consists in the surgical replacement of all skin layers, the so-called full-thickness skin transplantation. The indication of full-thickness skin transplantation in the acute care of surgical burn treatment has been limited. Full-thickness skin, consisting of epidermis and dermis, is particularly needed on mechanically stressed regions such as the palms of the hands and soles of the feet, and is saved for these areas of the body in third-degree burns.
Also, full-thickness skin grafting finds use in the therapy of cosmetically stigmatizing and function-restricting scars. Until now, the limiting factor in skin grafting was that it could not be transplanted over a large area and only at great expense.
With the new, innovative SkinDot full-thickness skin transplantation method, a surgical procedure is now available for the first time in which valuable full-thickness skin can be transplanted over a large area of the entire body.
Indication acute wounds
Bei akuten tiefen Wunden ersetzt das SkinDot Verfahren die komplette Haut durch Transplantation aller Hautschichten einschließlich der wichtigen Hautanhangsgebilde. So wird die natürliche Funktion gesunder Haut wiederhergestellt. Die Hautfunktion besteht aus:
- Haptile Funktion (Fühlen)
- Temperaturempfinden (Wärme- und Kältempfinden)
- Vibrationsempfinden
- Schmerzempfinden
- Talgdrüsenfunktion
- Schweißdrüsenfunktion
Akute Wunden sind definiert als plötzliche, meist durch einen Unfall entstandene Verletzungen von zuvor ungeschädigter Haut und Gewebe. Abhängig von ihrem Entstehungsmechanismus werden mehrere Arten von akuten Wunden unterschieden:
Risswunden: (Vulnus Lacerum)
Risswunden werden meist durch grobe Klingen von Kreissägen oder Fräsen verursacht. Sie zeichnen sich durch zerfetzte Wundränder aus und enthalten viele tote Gewebeanteile. Komplizierend treten häufig Verletzungen von Sehnen, Nerven oder anderer funktionalen Strukturen auf. Die Wundränder müssen meist neu angeschnitten und mittels Hautnaht versorgt werden. Nur wenn die Wundränder nicht spannungsfrei genäht werden können, ist eine Hauttransplantation notwendig.
Crush wounds (Vulnus Contusum)
Contusion wounds resulting from bilateral blunt force trauma are characterized by deep wound pockets with lacerated wound edges. Recovery of the destroyed tissue is usually impossible. Necrotic areas must be debrided and closed with sutures.
Crack-squeeze wounds (Vulnus Lacero-Contusum)
In the case of laceration-crush injury, there is usually no isolated accident mechanism, but a combination of several forces acting on the tissue. Lacerations are often caused by the action of high blunt force. Due to the combination of compressive, impact and tensile forces, the wound edges are usually irregularly lacerated and bloodshot. Radical surgical debridement is required for treatment, and the wound edges must be re-cut and sutured. If tissue tension is too high to allow wound closure by suturing alone, skin must be transplanted.
Lacerations (Vulnus scissum)
Lacerations are caused by sharp objects such as kitchen knives, razor blades or glass splinters. The wound edges are smooth and only slightly gaping. They tend to bleed profusely and can usually be treated – after wound cleansing – by suturing the skin. Careful assessment of symptoms can estimate the extent of damage to deep-seated structures. In the case of deep wounds and the possible presence of foreign bodies, surgical wound cleansing (debridement) is often performed before wound closure in the case of incised wounds.
Scrapes (Excoratio)
This superficial injury to the skin is caused by friction against rough surfaces, e.g. in a bicycle fall. Blood loss from these wounds is usually minor, but the often severe contamination requires thorough surgical cleaning. Skin suturing or skin grafting is not necessary.
Decolllement
Die Ablederung (Decollement) stellt einen Sonderfall der Schürfwunde dar. Durch tangential einwirkende Scherkräfte lösen sich Teile der Haut oder die komplette Haut ab und es entstehen große Wundareale. Als Ursache finden sich meist Überrolltraumen im Rahmen von Verkehrsunfällen oder schwere Motorradstürze bei hohen Geschwindigkeiten. Beim Decollement ist immer eine Hauttransplantation notwendig.
Stichwunden (Vulnus Ictum)
Stichwunden zeichnen sich durch meist kleine Einstichstellen aus, wodurch das Ausmaß der inneren Verletzungen oft unterschätzt wird. Aus diesem Grund ist eine sorgfältige Exploration des tiefen Gewebes bei dieser Art von Wunde unbedingt notwendig.
Bisswunden (Vulnus morsum)
Eine Bisswunde ist meist eine Kombination aus Stich-, Quetsch- und Risswunde mit dem Risiko der mikrobiellen Kontamination durch den Speichel des Verursachers. Eine Besonderheit in der Versorgung dieser Wunden besteht darin, dass sie seit Jahrhunderten offen behandelt wurden, d.h. eine Wundversorgung durch Naht obsolet war. Erst mit den neuen und sicheren Antibiotika können Bisswunden durch Naht versorgt werden. Dies erfolgt vornehmlich bei Bisswunden im Gesicht von Kindern. Bite wounds can have very small wound openings but often have significant depth extension.
In acute wound care, SkinDot is particularly suitable for loss of skin areas on the face, hands and feet, and over joint surfaces. Because the SkinDot procedure results in a stable full-thickness skin substitute, amputation stumps can be treated with SkinDot. The stable skin substitute protects against pressure points caused by the prosthesis, which often recur for years and are very painful.
Indication – Chronic wounds
The healing of skin wounds is a complex biological process that should take place as undisturbed as possible until it heals. A wound that does not heal over a period of three months is called chronic. Poor wound healing is often the result of a circulatory disorder, an immune defect, or diabetes mellitus.
A common chronic wound is the bedsore (decubitus ulcer). As long as the wound surface is not closed in fresh wounds, there is a risk of contamination of the wound by bacteria, viruses or fungi. Wound contamination can develop into the dreaded wound infection. Persistent wounds without wound closure can become chronic, resulting in a chronic wound. Chronic wounds result in a functionally and/or aesthetically very disruptive scar appearance due to delayed healing.
An important goal of surgical wound treatment, therefore, is to prevent wound infection and surgically restore the skin barrier in the wound area. But how can wound closure be accelerated?
There are numerous studies and publications on growth factors, stem cells, nanoparticles, various wound dressings, blood plasma, shock waves, etc. However, an effective, faster miracle closure could only be achieved by skin grafting.
The SkinDot procedure therefore not only prevents chronification of the wound through rapid wound closure, but is also one of the few effective treatment options for existing chronic wounds.
Indication – scar correction
If the number of regenerative skin cells (stem cells) in a wound is too low, the healing process is delayed. Originally healthy tissue is replaced by the body with defect tissue as part of the wound healing process. This inferior defect tissue is called scar tissue. Scar tissue is inelastic, has no skin functions such as sweat or sebaceous gland secretion, and therefore tends to be dry and sensitive.
When scars are cosmetically noticeable, patient distress can be very high, especially with stigmatizing scars on the face, forehead, décolleté, or back of the hand. Regardless of appearance, scars can also lead to functional limitations, especially if they are located over joint surfaces and lead to restricted movement. A special form of scar is the so-called “hypertrophic” scar, which is particularly raised and conspicuous. The duration of wound healing depends on the occurrence of hypertrophic scars. Wounds that do not heal completely within 21 days have a tendency to hypertrophy. Surgical scar therapy represents a classic indication for a so-called full-thickness skin graft. This full-thickness skin graft contains all skin layers with the epidermis and dermis.
With SkinDot, a new, innovative procedure is available in which scar tissue is replaced with hundreds of 1-3 mm full-thickness skin islands. These skin islands heal together, allowing the scar to be replaced with a skin graft that is comparable to healthy skin.
Your attending physician is not yet familiar with the new, innovative SkinDot procedure? Please inform him/her about the possibility of treating your skin wound with the new SkinDot procedure. We will be happy to advise you and perform the SkinDot procedure on you (if the indication is suitable). We look forward to your appointment!
Skin Transplantation beyond
Skin Transplantation 2.0