Your experts for skin transplantation
Hier erläutern wir Ihnen die verschiedenen Möglichkeiten der Hautverpflanzung. Lernen Sie die Vor- und Nachteile der SkinDot-Transplantation, Spalthaut-Transplantation, Kulturhautverfahren im Labor gezüchteter Zellen und die Möglichkeiten des Ersatzes tieferHautschichten (dermale Ersatzverfahren) kennen. Welche Hauttransplantation eignet sich wofür?
Ask our experts
Warning
They may contain disturbing photos.
Dermal replacement procedures
In deep wounds with complete loss of all skin layers, a dermal substitute matrix can be transplanted into the wound. This acts as a displacement layer. The dermis substitute must then be transplanted with split skin.
Culture skin method
Since the 1980s, skin cells can be cultivated in the laboratory. The skin cells cultivated in the laboratory can be transplanted onto the wound as so-called keratinocyte sheets or as a cell suspension.
Split skin graft
For extensive burns and superficial wounds, split-thickness skin grafting is the treatment of choice. Split skin is an ultra-thin skin graft of thickness up to 0.2 mm.
Full-thickness skin graft
In a deep wound with full-thickness skin loss, full-thickness skin grafting provides the best result. Full-thickness skin grafts are the most stable and contain all skin appendages.
Split skin graft
In the case of a loss of the epidermis, the deep (dermal) skin layer is completely or partially preserved, so that only a very thin skin layer in the form of the epidermis (split skin) must be transplanted. This type of injury occurs mainly in burn wounds (burn and scald IIb°). In the case of extensive burn wounds with loss of all skin layers, thin epidermis is also transplanted, since a full-layer replacement with full-thickness skin is not available over a large area. A maximum of 2-3% of the body surface can be replaced with full-thickness skin. Another possibility to replace the dermis consists of artificial dermal collagen constructs (see dermal replacement procedures), but these are very costly and complicated. Split skin is an ideal skin substitute if the dermis is preserved, but if the dermis is lost, it is only an inferior substitute for healthy skin. Split skin has a thickness of 0.2 mm and is mostly removed from the thigh. There, the split skin removal creates a kind of abrasion wound, which heals within about 14 days. There are three different techniques for split-thickness skin transplantation: the meshgraft technique, the sheetgraft technique and the Meek transplantation for extensive burns (see below).
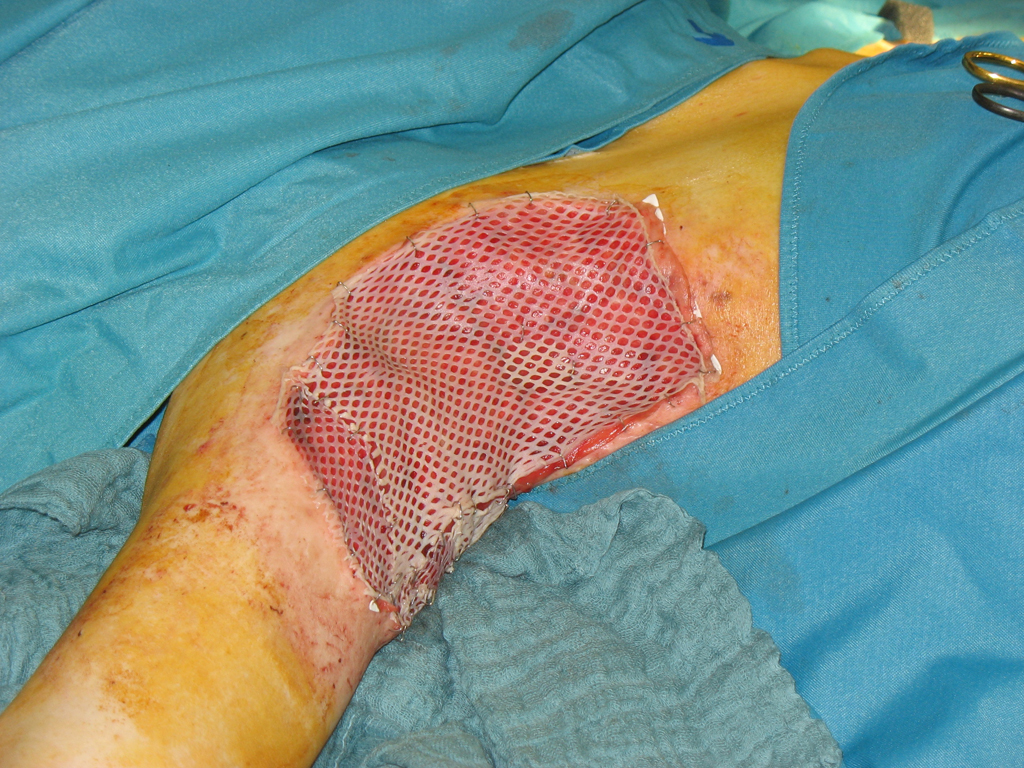
Meshgraft
In large burn wounds, the existing autologous skin must be expanded using various available techniques so that sufficient skin is available for wound closure. When the skin is processed by the mesh device, a mesh or net graft (meshgraft) results. This allows the area of the graft to expand at a ratio of 1:1.5, 1:3, 1:6 (in extreme cases up to 1:9). However, the greater the expansion, the longer and more prone to complications (wound infection) is the healing process. Since skin cells grow from the edges of the mesh grafts into the mesh gaps, the larger the mesh gaps, the longer healing takes. The major disadvantage of mesh grafting, especially in skin grafting after loss of the subcutaneous tissue (dermis), is the cosmetically and functionally unfavorable outcome.
The transplanted meshgraft skin tends to contract and shrink, resulting in scars, scar strands, and unstable scars. Not only can these scars be stigmatizing, but they can restrict movement via joint surfaces. Scar contraction on the neck is particularly dramatic with subsequent restriction of movement of the head. In addition, split skin grafts lack the shifting layer of the subcutis. The mesh structure of the mesh graft remains permanently visible. For these reasons, therefore, mesh graft transplantation in the face, décolleté, neck area and hands should be avoided if possible and reserved for severe burn victims. If the split skin has been grafted to wounds without subcutaneous tissue, persistent sensitivity and vulnerability of the grafted skin occurs due to loss of sweat and sebum secretion.
.
The guiding principle “Epidermis (epidermis) is life – dermis (subcutis) is quality of life” by the French burn surgeon Michel Rives has therefore lost none of its relevance.
| Meshgraft | Vorteil | Disadvantage |
|---|---|---|
| Skin quality of the graft | Poor, as no skin appendages in the graft, no stem cells present, no dermale Verschiebeschicht | |
| Healing of the graft | Since thin graft fast healing time | |
| Scarring | Grid or network structure visibler | |
| Donor area | Large-scale decrease at the thighs and on the back possible, but texture and pigment changes on the donor area | |
| OP-Zeit | First removal of the split skin and then transplantation, if necessary in parallel by two surgical teams |
Sheetgraft
If the extent and depth of the burn is limited to the epidermis, split skin (0.2 mm thickness) can be left in place for grafting and transplanted without EXPANSION. The size ratio is 1:1, and the graft is called a sheetgraft. Sheetgraft grafts are cosmetically favorable because these grafts do not result in a lattice or mesh pattern as with meshgraft, which occurs after the size expansion of the split skin (see above). Due to the limited removal possibilities, sheet graft grafts are used for particularly visible areas of the head (face, neck, décolleté, back of the hand). The main disadvantage here with meshgraft is the tendency to shrinkage, which all split skin grafts possess. Due to this contracture of the transplanted sheet grafts, the initially often excellent cosmetic and functional result is significantly reduced. Unfortunately, sheet grafting also results in scarring and scar contracture. Sheetgraft grafts are therefore suitable for surgical wound management in cases where the subcutaneous tissue is preserved and the wound areas are rather small.
| Sheetgraft | Vorteil | Disadvantage |
|---|---|---|
| Skin quality of the graft | Poor, as no skin appendages in the graft, no stem cells present, no dermal displacement layer | |
| Healing of the graft | Since thin graft fast healing time | |
| Scarring | Initially good, later often hypertrophic scarring especially at the margins, no Skin tags present | |
| Donor area | Large-scale decrease at the thighs and on the back possible, but texture and pigment changes on the donor area | |
| OP-Zeit | First removal of the split skin and then transplantation, if necessary in parallel by two surgical teams |
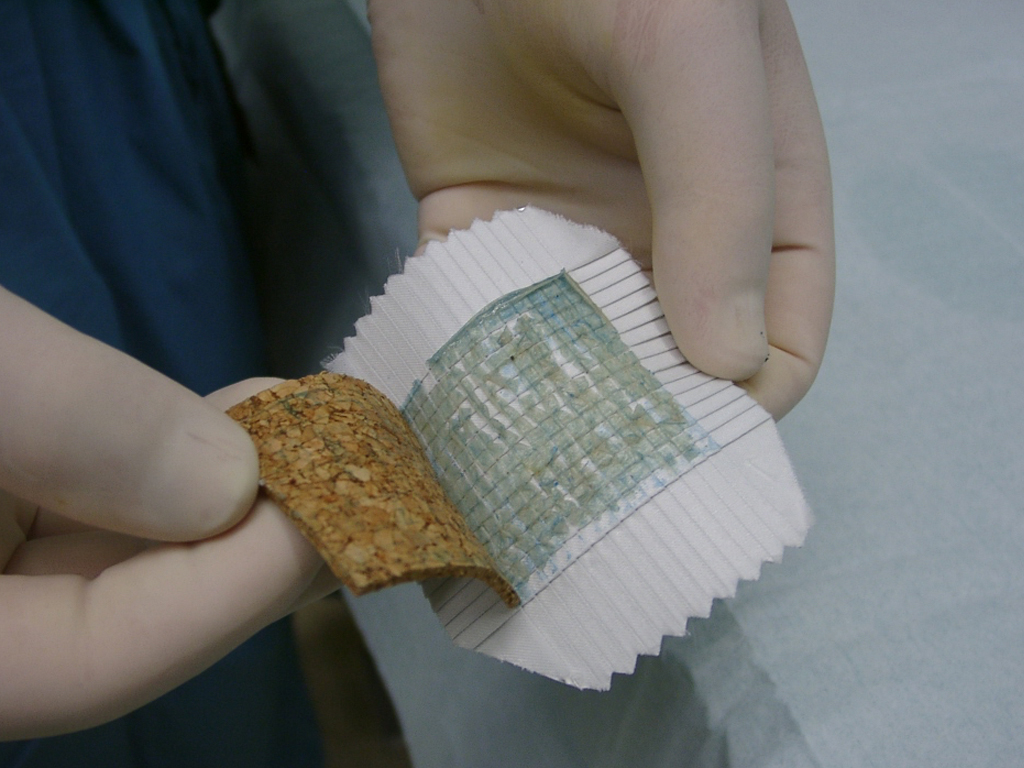
Meek technique
By meek or meekgraft technique is reserved for large area burns on the body. Also in the meekgraft technique, only the epidermis is transplanted, so it is split thickness skin. When using the Meek technique, the primary goal is to achieve rapid wound closure of the extensively injured skin and to save the life of the affected patient. Rapid wound closure is necessary because the lack of a skin barrier allows germs (bacteria, viruses and fungi) to enter the body with the risk of blood poisoning. With the Meek technique, wound care by split skin grafting is possible up to a burned body surface of up to 75% without. In modern burn surgery, for an even larger burned area of more than 75% of the body, additional skin cells cultivated in the laboratory are used (see tab “Cultivated skin techniques”). In addition, patients with extensive burns require numerous surgical procedures and several weeks of intensive medical treatment.
Advantages
Compared with the mesh technique, Meek grafting has several advantages for large-area burns. The most important advantage is that small and awkwardly located areas of the body can be used for split skin harvesting. Even with minimal healthy skin areas, it can be harvested for the marine technique. Another advantage is the easier handling of split skin expanded widely by Meek compared to the meshgraft technique, which is often fragile when expanded over a large area.
Disadvantages
Disadvantages are the high personnel requirement and a high time expenditure for the production of the Meek grafts. To avoid a long OR time, parallel surgery is performed by two surgical teams. While one team prepares the burn wounds for transplantation and removes the split skin, the second team working in parallel produces the Meek grafts.
| Meekgraft | Advantage | Disadvantage |
|---|---|---|
| Skin quality of the graft | Poor because no skin appendages in graft, no stem cells present, no dermal shift layer | |
| Healing of the graft | Since thin graft fast healing time | |
| Scarring | Island structure visible | |
| Donor area | Small area removal possible on all remaining healthy skin areas | |
| OP time | Complicated technique, long manufacturing time of the grafts necessary |
Your attending physician is not yet familiar with the new, innovative SkinDot procedure? Please inform him/her about the possibility of treating your skin wound with the new SkinDot procedure. We will be happy to advise you and perform the SkinDot procedure on you (if indicated). We look forward to hearing from you!
Skin Transplantation beyond
Skin Transplantation 2.0