Your Skin Transplant Experts
Deutscher Text: Hier erläutern wir Ihnen die verschiedenen Möglichkeiten der Hautverpflanzung. Lernen Sie die Vor- und Nachteile der SkinDot-Transplantation, Spalthaut-Transplantation, Kulturhautverfahren im Labor gezüchteter Zellen und die Möglichkeiten des Ersatzes tieferHautschichten (dermale Ersatzverfahren) kennen. Welche Hauttransplantation eignet sich wofür?
Ask our experts
Warning
They may contain disturbing photos.
Dermal replacement procedures
For deep wounds with complete loss of all skin layers, a collagen-based dermal substitute can be grafted into the wound. This collagen matrix acts as a skin shifting layer. A thin layer of skin must then be transplanted over the dermal substitute.
Culture skin method
Since the 1980s, skin cells can be grown in the laboratory. The skin cells grown (cultured) in the laboratory can be inserted into the wound as cell layers or sprayed on the wound.
Split skin graft
For extensive burns and very superficial wounds, so-called split-thickness skin grafting is the treatment of choice. Split skin consists of an ultra-thin skin graft of the thickness of only 0.2 mm.
SkinDot skin graft
In the case of a deep wound with a loss of the entire skin, skin replacement with so-called full-thickness skin provides the best result. Full-thickness skin grafts are very stable due to their dermal shifting layer and contain all skin appendages.
SkinDot Skin Graft
The first reports of full-thickness skin grafts date from ancient India, about 2500 to 3000 years ago. The first reports of skin grafts in modern times date from the second half of the 19th century (1872 Ollier, and 1875 Wolf, respectively). Other luminaries such as Reverdin (1899) and Davis (1910) established full-thickness skin transplantation.
By now, full-thickness skin grafting is an established routine method and should be safely mastered by every plastic surgeon. The donor region for a full-thickness skin graft should be as similar as possible in nature to the defect wound to be covered. Anatomically, a full-thickness skin graft, as the name implies, consists of the full-thickness skin of the epidermis and the dermis. The subcutis contains the skin appendages, such as hair roots, sebaceous glands, sweat glands and nerves. The varying density of the skin appendages should be taken into account when choosing the site for removal of the full-thickness skin.
In particular, undesirable hair growth resulting at the wound (recipient site) should be avoided, iespecially in facial transplantation. A healed full-thickness skin graft can sweat just like healthy skin. Regular oiling is also not necessary (in contrast to grafting through thin epidermis), because the sebaceous glands are present in the full-thickness skin graft. Full-thickness skin is also much thicker than the thin epidermis and thus provides a shifting layer and corresponding stability.
While the thin epidermis (split skin) is very sensitive, full thickness skin can be loaded accordingly. Full-thickness skin is therefore particularly suitable for transplantation in the face, décolleté, hands, feet, over joint surfaces and on the amputation stump. After removal of the thin epidermis results in a kind of abrasion, the thin epidermis is replaced within about 14 days by the stem cells contained in the deep skin layer.
.
In contrast, the removal of full-thickness epidermis results in skin gaps that must be sutured closed by staggering the surrounding skin. This circumstance explains why only small full-thickness skin grafts can be harvested. Until now, a maximum of 2-3% of the body surface could be replaced with full-thickness skin grafts. This problem is solved by the new SkinDot procedure.
In SkinDot transplantation, countless 1 – 3 mm full-thickness skin islands are inserted into the wound. The 1 – 3 mm skin gaps created at the donor site heal with hardly any visible complications. The extracted islands of full-thickness skin are then transplanted into the wound by the SkinDiot procedure, so that new multi-layered skin is created there from the hundreds of millimeter-sized islands.
Healing of the full-thickness skin graft
.
The healing of full-thickness skin grafts, both the previous small full-thickness skin grafts and the SkinDot full-thickness skin islets, takes place as the smallest blood vessels (arteries and veins) sprout from the wound bed into the graft. The graft is supplied with blood and nourishment through the new vascular connection. Veins and lymphatic vessels as well as nerves also sprout into the full-thickness skin graft or SkinDot islets during the healing process. Blood vessels take only 4-5 days to sprout, while nerves can take several months to sprout. The blood vessels that sprout into the graft are called capillaries (Latin capillus = hair) because they are thinner than hair. This capillary sprouting is very fragile after transplantation, which is why the graft must be protected from movement and shear forces. Therefore, in the SkinDot procedure, a special sponge is placed on the small millimeter-sized islands to create a negative pressure. This negative pressure protects the graft from movement and shear forces, thus ensuring that the SkinDot full-thickness skin islets heal safely. SkinDot grafting transplants all layers of skin into the wound, resulting in a particularly stable and functional skin graft.
Indication for SkinDot Skin Graft
.
Die Indikation für ein Vollhauttransplantat besteht immer dann, wenn ein besonders stabiles Hauttransplantat erforderlich ist. Nur Vollhauttransplantate besitzen eine der gesunden Haut vergleichbare Qualität. Im Gegensatz zu dünnen Hauttransplantaten (Spalthaut) besitzen SkinDot Transplantate nur eine minimale Schrumpfungstendenz. Dies Schrumpfungstendenz von Spalthauttransplantaten führt zu den sogenannten Narbenkontrakturen, die kosmetisch extrem ungünstig und bewegungseinschränkend sein können.
Klassische Indikationen für Defektdeckungen durch SkinDot Vollhauttransplantate sind:
- Tiefe Defektwunden im Gesicht und Stirn (z.B. nach Tumorentfernung oder Brandwunden)
- Tiefe Vollhautwunden an Händen und Füßen
- Unfallbedingter Hautverlust über Gelenkflächen
- Notwendiger Hautersatz am Amputationsstumpf (Belastungszone)
- Deckung von chronischen Wunden
- Narbenkorrekturen
Operative Procedure for SkinDot Skin Graft
.
In the new, innovative SkinDot procedure, the suitable body area is first selected with the patient, from which the countless small, millimeter-sized skin islands are removed (donor area). The donor area should be as identical as possible in skin texture to the wound to be transplanted. For example, if a replacement of full-thickness skin (full-thickness skin) is needed in the right palm, the left palm is selected as the donor area. Only in the opposite hand will the skin have a comparable consistency, thickness and quality as in the injured hand. In case of a deep defect wound on the cheek, 1 mm skin is taken from the other side of the cheek. On the thigh or lower leg, on the opposite side in each case. This procedure results in a so-called full thickness skin equivalent, i.e. the transplanted skin is comparable to the original skin that is to be replaced. After the SkinDot full-thickness skin islands have been harvested, the surgeon inserts them into a collagen matrix. In this process, the SkinDot islands are only 1 – 2 mm apart in the matrix, so that the layers in the transplanted SkinDot islands can grow together undisturbed.
After the islets are placed in the matrix (with the skin islets inside), they are transplanted into the wound. A negative pressure dressing is applied over the graft to ensure safe healing.
This negative pressure dressing remains on the transplanted wound for approximately 10 days to protect the full-thickness skin islands from shear forces and to ensure undisturbed sprouting of the blood vessels.
Recipient and donor area
.
Gesicht:
Da die entnommenen SkinDot Vollhautinseln den Hautverlust in der Defektwunde nahezu identisch ersetzen sollen, werden die Hauptinseln im unmittelbar angrenzenden Gesichtsbereich entnommen. Entnahme der Hautinseln bei einer Wunde an der Stirn daher an der Stirn, bei Hautverlust an der Wange an der gegenüberliegenden Wange usw. Die transplantierten Hautinseln im Gesicht haben eine Größe von maximal 1 mm, die durch die Abnahme entstandenen 1 mm großen Hautlücken unauffällig und kaum sichtbar verheilen. An der Abnahmestelle kann es mitunter zu Pigmentverschiebungen kommen, d.h. es können helle oder dunkle 1 mm große Punkte sichtbar sein, die wie Sommersprossen anmuten.
Décolleté:
Bei einer SkinDot Transplantation im Décolleté Bereich werden die Inseln am Décolleté entnommen. Das Prinzip der SkinDot Hauttransplantation besteht darin, dass die Inseln unmittelbar in der Nachbarschaft der Wunde entnommen werden, da nur dort die Haut das gleiche Aussehen und die gleiche Qualität wie in dem Wunddefekt besitzt.
Gelenkflächen:
Über Gelenkflächen ist ein stabiles und belastbares Vollhauttransplantat erforderlich. Nur Vollhauttransplantate besitzen keine Kontrakturneigung, d.h. sie schrumpfen im Gegensatz zu anderen Hauttransplantaten nicht zusammen. This shrinkage often results in restricted joint motion in alternative grafting procedures. The contracture tendency of thin skin grafts is particularly evident in the neck region, so that massive movement restrictions of the head can occur here.
Hände und Füße:
Die Haut des menschlichen Körpers hat an den Handflächen und Fußsohlen ihre maximale Belastbar- und Zugfestigkeit. Diese äußert sich bei wiederholter Belastung durch sogenannte Schwielen. Verluste des Hautmantels in diesen Bereichen führen oftmals beim Ersatz durch dünne Hauttransplantate (Spalthaut) zu massiven Einschränkungen im Alltag. Dünne Hauttransplantate sind sehr empfindlich und neigen zu kleinen Verletzungen, die sich besonders an den Händen und Füßen schnell entzünden. Durch die Entnahme der SkinDot Vollhautinseln an der gegenüberliegenden Hand bzw. Fuß resultiert ein stabiles und belastbares Vollhauttransplantat, das mit der originären Haut vergleichbar ist.
Hautverlust am Köperstamm:
Auch hier gilt, dass die transplantierte Haut eine vergleichbare Konsistenz, Dicke und Qualität haben sollte. Die Zahl der Hautanhangsgebilde ist je nach Köperareal sehr unterschiedlich. Die Haut hat im Nacken eine ganz andere Dicke als z.B. am Schienbein. Mit dem SkinDot Verfahren wird bei Hautverlust im Nacken der Defekt nur durch Hautinseln ersetzt, die auch im Nacken entnommen wurden. Bei Vollhautwunden am Scheinbein werden die Inseln, abhängig von der Wundgröße, nur am betroffenen Schienbein und/oder dem gegenüberliegenden Schienbein entnommen. Nur beim SkinDot Verfahren ist daher ein vergleichbarer Hautersatz im Empfängerareal gewährleistet.
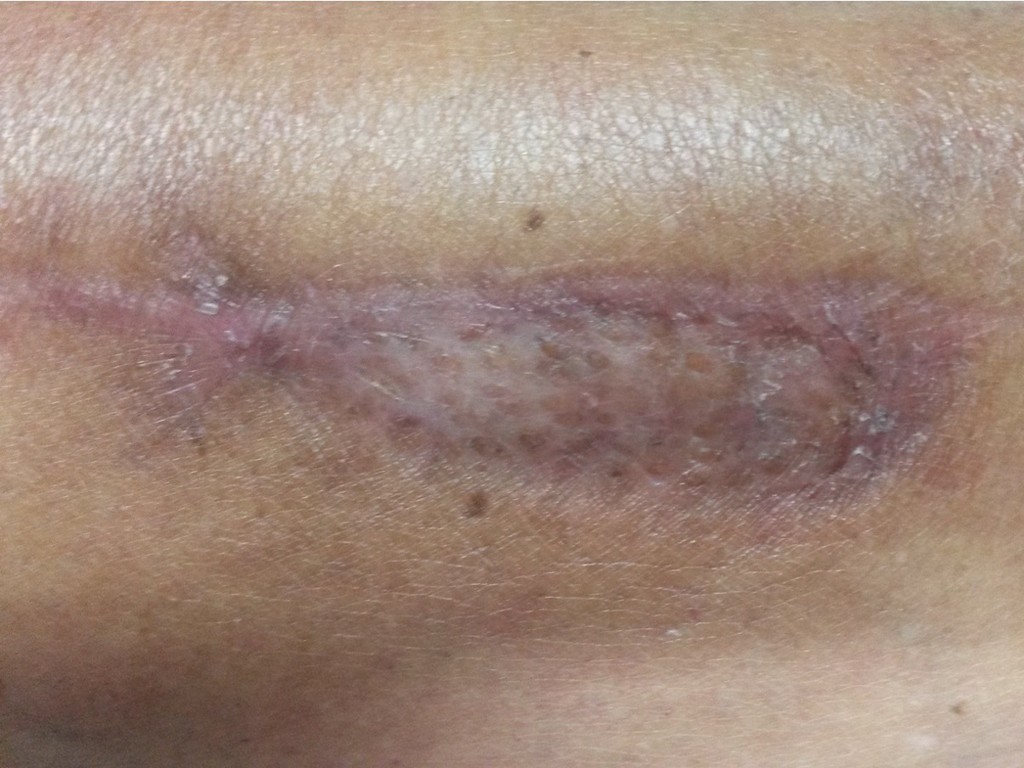
Operating result
The results after SkinDot skin grafting vary greatly from individual to individual and depend on wound location, previous diseases, skin type and color as well as patient age. Wound healing is a complex, multifactorial physiologic process that occurs differently in each individual. The cosmetic and functional results to date after SkinDot transplantation are very promising. Minimal scarring results and a very thick, stable and resilient skin graft. However, it would be unscientific and unfair to promise a skin substitute that is 100% like healthy skin. Compared to previous skin grafting procedures, however, the SkinDot procedure stands out because it closely resembles healthy skin and is superior to previous skin grafting procedures.
Your attending physician is not yet familiar with the new, innovative SkinDot procedure? Please inform him/her about the possibility of treating your skin wound with the new SkinDot procedure. We will be happy to advise you and perform the SkinDot procedure on you (if the indication is suitable). We look forward to your appointment!
Skin Transplantation beyond
Skin Transplantation 2.0